Stress Management
Introduction
Chronic stress is a relentless companion in our modern lives, affecting our physical and mental well-being in ways we often underestimate. While its psychological toll is well-documented, there’s an intricate web of connections between stress and physical ailments that remains largely unexplored. In this journey through the world of somatics, we’ll delve into a topic that’s often overlooked: the profound link between chronic stress and heartburn.
Heartburn, that burning sensation in the chest and throat, is a familiar discomfort for many. We’ve all experienced it at some point, often attributing it to spicy foods or overindulgence. But what if I told you that heartburn might be more than just an occasional annoyance? It can be a silent signal from your body, a red flag waving in the face of chronic stress.
In this blog post, we’re going to unravel the intricate relationship between chronic stress and heartburn. Beyond the surface, we’ll uncover the lesser-known physical symptoms that heartburn can trigger and explore how these often obscure indicators can lead to misdiagnoses and prolonged suffering. But don’t worry; we won’t leave you hanging. We’ll also dive into the world of somatic solutions, offering holistic approaches to alleviate both chronic stress and heartburn. So, fasten your seatbelts as we embark on this enlightening journey through the realms of stress, somatics, and the secret language of heartburn.
The Fire Within: Understanding Heartburn's Burning Grip
Heartburn, often described as a fiery sensation in the upper chest or throat, isn’t just an annoyance; it’s a full-blown sensory assault. The culprit? Stomach acid backing up into the esophagus, the tube connecting your mouth to your stomach. This acidic invasion triggers a range of physical symptoms:
- Burning pain or discomfort: This hallmark symptom can range from a mild prickling to a searing sensation in the chest, throat, or even jaw.
- Chest tightness or pressure: The burning sensation can be accompanied by a feeling of tightness or pressure in the chest, mimicking the discomfort of angina or a heart attack.
- Sour taste or belching: As stomach acid rises, it can leave a sour or bitter taste in your mouth, along with an unpleasant urge to belch.
- Difficulty swallowing: The inflamed esophagus can make swallowing uncomfortable, further adding to the distress.
- Ear & sinus pain: While less common, some individuals experience earaches and sinus pain due to the shared nerve pathways connected to the esophagus.
- Dyspnea (difficulty breathing): In rare cases, severe heartburn can trigger a feeling of shortness of breath, adding to the anxiety and discomfort.
Did you know that one in four Americans experiences heartburn at least once a week, according to the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK)? That’s a staggering number, indicating just how common this fiery discomfort is.
But the trouble doesn’t stop there. These uncomfortable symptoms can easily be misinterpreted, especially for those prone to anxiety. The chest tightness and pressure can mimic the warning signs of a heart attack, leading to panic and a surge of adrenaline. This heightened anxiety, in turn, can further disrupt digestion, creating a vicious cycle that intensifies both the heartburn and the anxiety. A study published in the Journal of Clinical Gastroenterology found that individuals with anxiety disorders were twice as likely to experience heartburn compared to those without anxiety.
This isn’t just a theoretical connection; it’s a physiological reality. When we experience stress or anxiety, our bodies release hormones like cortisol, which can slow down digestion and weaken the lower esophageal sphincter, the valve that keeps stomach acid down. This creates a perfect storm for heartburn, and the discomfort fuels the anxiety further, perpetuating the cycle.
So, the burning sensation you experience isn’t just physical; it’s often intertwined with a complex interplay of physiology and emotions. Understanding this connection is crucial, as it empowers you to address the root cause and break free from the cycle of stress-induced heartburn and anxiety.
The Acidic Myth: Debunking the Stress-Heartburn Connection
For decades, the conventional wisdom blamed heartburn on one culprit: excess stomach acid. Pop antacids and reduce spicy foods, they said, and you’ll be back to normal. But what if the story isn’t quite so simple?
Recent research throws a wrench in the acidic myth, suggesting that stress can play a major role in triggering heartburn, even with normal acid levels. This may seem counterintuitive, but it highlights the complex interplay between our minds and bodies.
Myth Busters: While excess stomach acid can certainly contribute to heartburn, research suggests it’s not always the primary culprit. Studies have shown that individuals with normal acid levels can still experience significant heartburn during stressful periods. This indicates that other factors are at play. In fact, I’m a perfect example of this persona. When I experienced two years worth of heartburn, I went to countless doctors, who ran countless tests, only to find out that there was nothing functionally wrong with me.
Stress: The Silent Saboteur
So, how does stress wreak havoc on our digestion? Buckle up, because the answer involves a multi-pronged attack on our digestive system:
- Digestive Downturn: When stressed, our bodies prioritize “fight or flight” responses, diverting resources away from digestion. This can lead to slowed down digestion, allowing stomach acid to linger and irritate the esophagus.
- Sensitive to the Burn: Stress can also increase our sensitivity to acid, even if the actual acid levels are normal. This means we perceive even small amounts of acid as more intense, amplifying the burning sensation.
- Sphincter on Strike: The lower esophageal sphincter, the muscular valve keeping stomach acid down, can be weakened by stress hormones. This creates a leaky barrier, allowing acid to creep up into the esophagus and ignite the fire.
- Gut Bacteria Blues: Chronic stress can disrupt the delicate balance of gut bacteria, which plays a crucial role in digestion. This imbalance can contribute to inflammation and irritation, further fueling the heartburn flames.
The takeaway? Stress isn’t just a mental burden; it can wreak havoc on our digestive system, contributing to heartburn even in the absence of excess acid. Understanding this mind-body connection empowers us to address the root cause of the discomfort and seek solutions beyond just neutralizing acid.
Stress as the Culprit: Evidence for the Mind-Body Connection
As humans, we often gravitate towards the simplest explanation, the quickest fix. When it comes to heartburn, this often translates to popping antacids and hoping for the best. But what if the true culprit isn’t as readily apparent, lurking beneath the surface of our immediate assumptions?
The truth is, heartburn remains an enigma, a complex puzzle with many pieces yet to be fully understood. This very uncertainty, however, can lead doctors to prioritize readily identifiable and treatable “functional” issues, overlooking the bigger picture: the interconnectedness of our mind and body. This is where functional medicine shines, offering a holistic approach that delves deeper, recognizing the potential for stress to be the hidden hand behind the fiery discomfort, even when acid levels appear normal.
The Evidence Beyond the Acid
While the traditional narrative points to excess stomach acid as the primary culprit, research paints a different picture. Studies like the one published in Gut highlight a significant correlation between major life stressors and increased heartburn, suggesting that chronic stress can be a major trigger. Another study in Alimentary Pharmacology & Therapeutics reveals a direct link between perceived stress levels and the severity of heartburn symptoms, emphasizing the role of individual experience in shaping our physical response.
The Nervous System: The Conductor of Digestion
Our bodies are intricately wired, and the nervous system plays a crucial role in orchestrating various functions, including digestion. The vagus nerve, part of the parasympathetic nervous system, acts as the “relaxation response” pathway, promoting digestive processes. However, when stress takes hold, the sympathetic nervous system, responsible for the “fight or flight” response, kicks in. This triggers a cascade of changes:
- Digestion slows down: Blood flow is diverted away from the digestive system, leading to sluggish digestion and increased acid exposure in the stomach.
- Sensitivity to acid rises: Stress hormones can make the esophageal lining more sensitive to acid, even in normal amounts, amplifying the burning sensation.
- Sphincter weakens: The lower esophageal sphincter, responsible for keeping stomach acid down, relaxes under stress hormones, creating a leaky barrier and allowing acid to reflux.
The Gut-Brain Axis: A Two-Way Street
The gut and brain are constantly communicating through a complex network known as the gut-brain axis. This bidirectional communication means that stress can impact gut health, and gut issues can, in turn, influence mood and anxiety. Chronic stress can disrupt the gut microbiome, the community of bacteria residing in our intestines. This imbalance can contribute to inflammation, irritation, and altered gut motility, all of which can contribute to heartburn.
The takeaway? Stress isn’t just an emotional burden; it’s a physiological one that can significantly impact our digestive system and contribute to heartburn, even in the absence of excess stomach acid. Recognizing this mind-body connection empowers us to explore stress management strategies as part of our heartburn relief plan.
Beyond the Band-Aid: Seeking the Right Help for Heartburn's Hidden Cause
Let me be honest, I know heartburn all too well. It wasn’t always the fiery beast it became. It started subtly, an occasional twinge after a stressful day. But as burnout took hold, so did the heartburn, evolving into a two-year chronic issue that left me breathless and bewildered.
My journey began like many others. The primary doctor chalked it up to anxiety and offered to prescribe medication that felt like treating a symptom, not the root cause. Determined to find relief, I dove into the world of diets, meticulously eliminating “acidic” foods. It offered fleeting comfort, but the burning embers remained. Furthermore, it turned into a borderline obsession that had me teetering into the world of health anxiety.
Next came the gastroenterologist and the dreaded upper endoscopy. The verdict: gastritis. Armed with a new label and a strict low-acid diet, I soldiered on. Yet, the discomfort persisted, morphing into full-blown dyspnea, leaving me gasping for air, anxiety swirling in my chest.
The chest pain, mimicking a heart attack, landed me in urgent care and the ER three times a week. Each visit felt like a desperate plea for answers, leaving me frustrated and empty-handed. Then, during yet another urgent care visit, a doctor mentioned Pepsin GI, a digestive enzyme. It sounded unconventional, but desperation fueled my hope. And wouldn’t you know it, the fire in my chest extinguished almost instantly.
This unexpected relief sparked a deeper curiosity. I delved into research, discovering the power of zinc in aiding digestion. This led me to a homeopathic doctor who, unlike the others, saw the bigger picture. She recognized the stress lurking beneath the surface, the hidden culprit orchestrating the symphony of discomfort. With her guidance, I addressed the stress, not just the heartburn, and finally, the healing began.
This experience taught me a valuable lesson: sometimes, the most effective treatment doesn’t come in a pill or a strict dietary restriction. It lies in understanding the interconnectedness of our mind and body, seeking solutions that address the root cause, not just the presenting symptom.
So, when should you seek professional help? If your heartburn persists despite lifestyle changes, if it disrupts your sleep, or if you experience any concerning symptoms like dysphagia or chest pain radiating to your jaw, don’t hesitate. Remember, you’re not alone in this journey. Talk to your doctor, explore different approaches, and advocate for your own health. The key? Finding a practitioner who listens, who delves beyond the surface, and who recognizes the potential for stress and other underlying factors to be the hidden players behind your discomfort.
This isn’t just about finding relief from heartburn; it’s about embracing a holistic approach to your well-being, one that empowers you to heal your body and mind, together.
Taming the Flame: Stress Management for Heartburn Relief
Staring down the fiery discomfort of heartburn doesn’t have to be a solo battle. By incorporating stress management practices into your daily routine, you can empower yourself to find lasting relief and quell the flames from within. Here are some powerful tools to add to your arsenal:
1. Mindfulness & Meditation: Train your mind to be present and observe stress without reacting. Practices like mindfulness meditation can help you detach from stressful thoughts and cultivate inner peace, ultimately reducing the physiological impact of stress on your digestion.
2. Deep Breathing Exercises: Diaphragmatic breathing activates the relaxation response, slowing your heart rate and easing digestive discomfort. Simple techniques like box breathing (inhaling for 4 counts, holding for 4, exhaling for 4, holding for 4) can be practiced anywhere, anytime.
3. Yoga & Relaxation Techniques: Unwind your body and mind with yoga stretches, progressive muscle relaxation, or guided imagery. These practices can help release physical tension and soothe your nervous system, creating a calmer internal environment for digestion. Yoga with Adrienne has an incredible video that aids with digestion (my go-to when I experience the occasional bout of heartburn to this day).
4. Journaling & Emotional Expression: Bottling up emotions can exacerbate stress. Journaling allows you to express your feelings in a safe space, while talking to a trusted friend or therapist can provide valuable emotional support and stress management strategies.
5. Healthy Lifestyle Modifications: Prioritize quality sleep, regular exercise, and a balanced diet rich in fruits, vegetables, and whole grains. These practices promote overall well-being, reducing inflammation and creating a foundation for optimal digestion.
Remember, identifying and addressing your personal stressors is crucial. What triggers your anxiety? What work patterns contribute to burnout? Recognizing these factors empowers you to make adjustments in your life, reducing the overall stress burden and creating a more supportive environment for your gut health.
Healing the Gut: While addressing stress is key, sometimes damage has already been done to the gut lining. In such cases, temporary support with specific products can be beneficial. Consider exploring options like:
- Doctor’s Best Pepzin GI: This digestive enzyme blend can aid in the breakdown of proteins, easing discomfort and promoting smoother digestion.
- Reflux Gourmet: This supplement combines essential vitamins, minerals, and herbs known to support gut health and reduce inflammation.
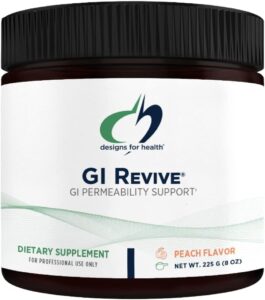
- GI Revive: Consider including Designs for Health GI Revive, a supplement containing L-glutamine and other gut-supportive ingredients, alongside stress management strategies to aid in healing your stomach lining and alleviate heartburn.
Disclaimer: This information is for educational purposes only and does not constitute medical advice. Please consult with your healthcare professional before starting any new supplements or treatments. As an Amazon Associate I earn from qualifying purchases
Remember, finding relief from heartburn is a journey, not a destination. By embracing stress management, incorporating healthy habits, and exploring potential supportive products, you can empower yourself to tame the flames and reclaim your digestive peace of mind.
Conclusion
The journey through the fiery maze of stress-induced heartburn can feel isolating and overwhelming. But remember, dear reader, you are not alone. This post has hopefully shed light on a hidden truth: stress can be a major player in this discomfort, even when acid levels seem normal.
Understanding the mind-body connection empowers us to move beyond quick fixes and embrace a holistic approach. By incorporating stress management techniques like mindfulness, deep breathing, and healthy lifestyle modifications, we can create a calmer internal environment for optimal digestion. Additionally, exploring supportive products under the guidance of your healthcare professional can offer temporary assistance on the healing path.
Remember, healing is a journey, not a destination. There will be setbacks, moments of frustration, and days when the fire seems to reignite. But armed with knowledge, self-compassion, and a commitment to stress management, you can reclaim control of your well-being.
SHARE
THREADS

Caroline
As a tech industry professional, Caroline experienced the detrimental effects of burnout and chronic pain firsthand. Motivated by her own journey, she now dedicates herself to assisting others in finding resources and support.
Related
Caroline Who?

As tech industry professional, Caroline experienced the detrimental effects of burnout and chronic pain firsthand. Motivated by her own journey, she now dedicates herself to assisting others in finding resources and support. Through The Happy Soup, Caroline shares resources and personal stories, providing a roadmap for recovery and offering a guiding hand to those facing similar challenges. With a compassionate approach, she inspires individuals to reclaim their lives, emphasizing that they are not alone in their struggles.